SARS-CoV2 Novel Coronavirus
The content on this newsletter is for educational purposes only and should not be used as a substitute for medical advice. Please consult with your healthcare provider ASAP if you develop symptoms.
Key Points
- Practice meticulous hygiene and social distancing.
- The U.S. will likely have significant levels of transmission increase in the next 1-2 weeks that may require quarantine/lock-down measures implemented by the local government.
- We may be in this for the long haul so if you are at low risk, start to think about how to continue your life and tend to necessary tasks while being mindful of the pandemic.
- At Tupelo Pointe, we always sanitize with industrial grade medical cleanser between patients and are even more meticulous about this on frequently used surfaces given the recent pandemic. This is a very low risk environment given the small and exclusive panel of patients in the practice with only 3-4 patients coming through on a given day. If you need to push back upcoming appointments, please do not hesitate to contact me.
- Continue good health practices by taking your vitamins, engaging in clean eating, exercise, and sleep. If you are out of vitamins or want to switch to recommended brands, please contact me.
- If you develop cold or flu symptoms, don’t panic. You probably have the common cold and should practice good hygiene to protect others.
- More information is coming out about the SARS-CoV2 virus/COVID-19. There is still a lot we don’t know.
Fact vs. Fiction
- You should be concerned about COVID-19 for a variety of reasons stipulated below.
- Wear a surgical face mask to protect yourself and others from droplet and cough transmission and to remind yourself from touching your face.
- Practice meticulous hygiene. Wash your hands often. Avoid touching your face.
- Stay away from people at high risk to protect them from YOU.
- You will probably contract SARS-CoV2 and have none to mild symptoms.
- There are no natural remedies or preventative remedies currently available for the treatment or prevention of COVID-19.
Why you should care
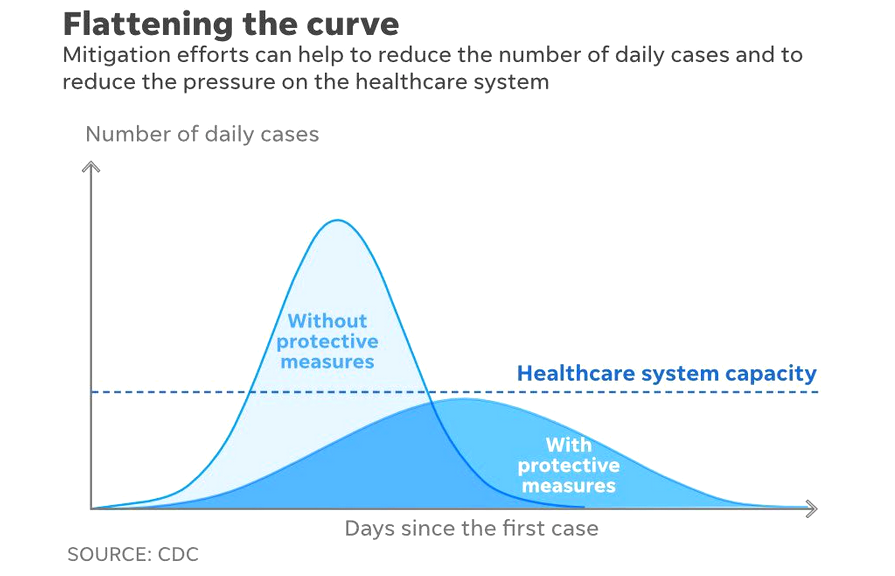
- We need to flatten the curve of severely infected patients so they have an increased chance of survival.1
o If we slow down the rate of infection, we avoid overwhelming the limited number of hospital beds, ICU beds, and healthcare workers in your community.
o The longer you or your neighbors can hold out before becoming infected, the more time you give researchers to come out with treatments.
The Virus
- SARS-CoV2 is the name of the virus; COVID-19 is the disease caused by the virus.
- SARS-CoV2 is called a novel virus because the strain has never been seen and the human immune system has not been exposed to it.
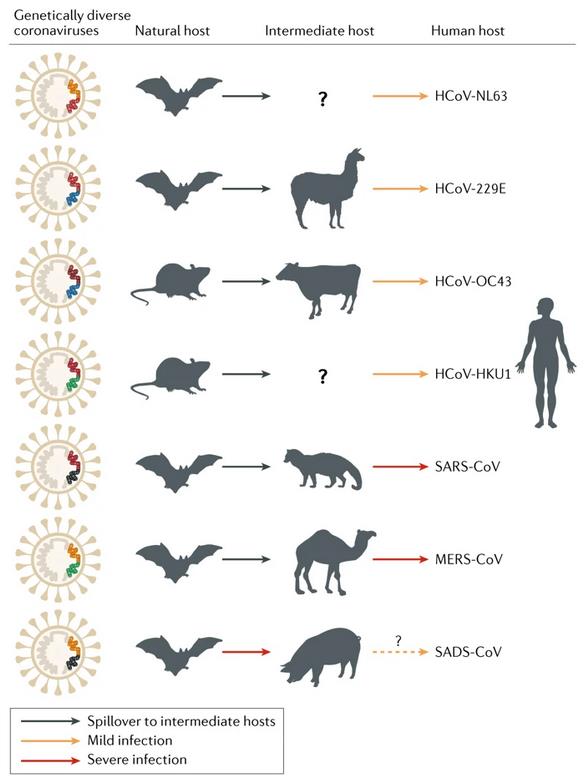
o SARS-CoV2 is likely transmitted from a bat to pangolin to human at an illegal “wet” market.2
- This is the 3rd epidemic caused by a coronavirus in the last 30 years.2,3
o The SARS-CoV1 caused the first epidemic of coronavirus, Severe Acute Respiratory Syndrome (SARS), in Asia in 2002.
o MERS-CoV caused the second epidemic of coronavirus, Middle East Respiratory Syndrome (MERS), in Saudi Arabia in 2010.
o Going forward, epidemiologist believe there may be one of these epidemics/pandemics every decade that will originate from one of these “wet” markets.
Pathophysiology
- SARS-CoV2 virus invades cells through the Angiotensin‐converting enzyme 2 (ACE2) receptor.4
- The virus attacks lungs (type II alveolar cells), kidneys, blood vessels, heart, GI tract where ACE2 receptors are found.
o This may account for the large number of heart attacks that are associated with SARS-CoV2.5
o The virus also attacks the GI tract in 10% of hospitalized patients with the SARS-CoV2.5 These symptoms are diarrhea and vomiting.
- If you are on ACE-inhibitors or ARBs, stay on them unless specified by your doctor.
Populations at risk6
- COVID-19 is particularly lethal for certain population groups.
- Children and adolescents don’t seem to get sick, but are carriers.7
- Some people do not get sick, but are carriers.
- The most vulnerable people have approximately 10-20% fatality rate and have one or more of the following:
o Over the age of 70-years-old
o Those with heart disease (15% of hospitalized cases), hypertension (15-30% of hospitalized cases), diabetes mellitus (12-20% of hospitalized cases) 5,8
o The immunosuppressed
o Healthcare worker/first responders – 15% of healthcare workers tend to develop a more severe version of the virus despite other risk factors
Lethality/Transmission
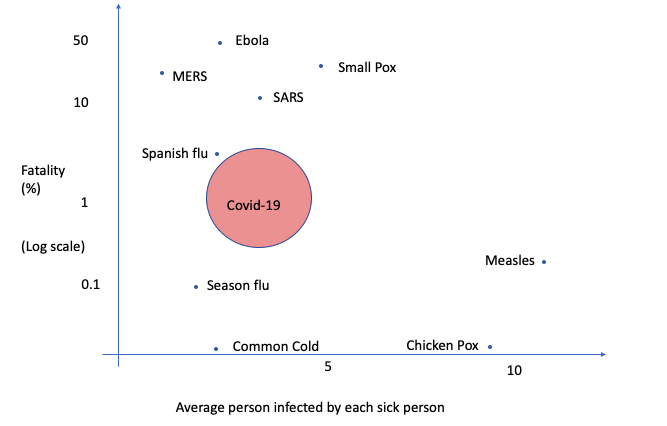
- Exact numbers are not known, but most Epidemiologist/Infectious Disease experts believe that the spread is anywhere from 2.24-3.58 persons who get infected from a single infected individual.9
o Many people do not get sick but are carriers, so the disease is easy to spread.
o The virus can live on surfaces for 8-72 hours.10
- Covid-19 has an estimate of 0.6% -3.4% fatality rate, 4-20x higher than influenza.6
- The reported numbers are underestimates. Likely for every reported case, there are 100 people who have been infected.
- We don’t know how SARS-CoV2 is transmitted. Some identified modes of transmission are microdroplets on surface, directly onto someone from coughing, airborne, and fecal.11
- Current CDC guidelines recommend contact and droplet protection. Aerosol protection with a N95 mask is recommended for high risk procedures where aerosolization may occur.1
- Currently we are seeing the following aerosol and surface stability of SARS-CoV2:10
o aerosols, up to 3 hours post aerosolization
o up to 4 hours on copper
o up to 24 hours on cardboard
o up to 2-3 days on plastic and stainless steel
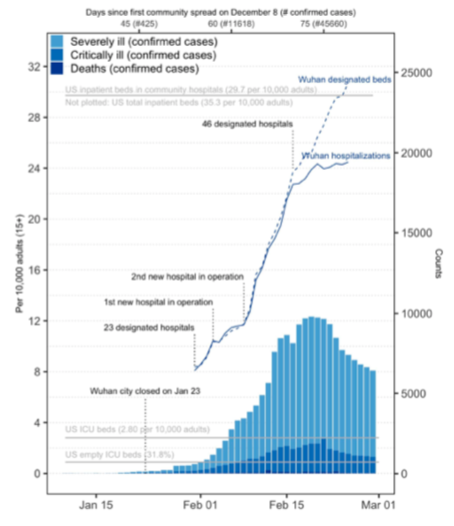
Healthcare Capacity
- The US has likely been too late to respond in terms of a PUBLIC HEALTH crisis.12
o This is according to Peter Hotez M.D., Ph.D., dean for the National School of Tropical Medicine Baylor College of Medicine
o The US will now start to test and we will see a large increase in the level of community transmission in the next 1-2 weeks.
o Likely community spread in the US started approximately February 22.12
§ Since January with the announcement of the outbreak in China, I have been monitoring the situation, practicing contact precautions in the hospital clinics and public areas, and communicating with colleagues in ground zero about the outbreak.
§ There was much misinformation and unknowns until the last few weeks as confirmable information started to come out in the scientific and medical community.
- Practice social distancing to slow down the spread of COVID-19.1
o This allows for us to flatten the curve and not overwhelm the healthcare system.
o Likely we will all become infected and those at risk will develop serious disease, but if we slow the rate at which we develop the disease, the healthcare system will have resources available to take care of you.
o 5% who develop COVID-19 and are hospitalized require ICU level care with ventilation up to 6 weeks. The US as a nation has one of the fewest numbers of ICU beds per capita.13
- Healthcare capacity and the overwhelming of beds is not theoretical and it occurred in Italy and has resulted in a reported 6% death rate for COVID-19 as opposed to China with a reported 2% death rate.13
How to protect yourself and loved ones
- Do not engage in long-term fasting defined as >24-48 hours of fasting. Continued timed eating if you already do this.
o There is a transient dip in the immunity with longer fasting times followed by an increase in immunity after refeeding.14
- Continue to take your supplements and medications as prescribed to maintain your current immune health.
o Do not increase or decrease your medications without talking to your doctor.
o There is absolutely no evidence or reports that any specific supplementation or regimen protects against a novel virus.15
o COVID-19 causes inappropriate immune response including cytokine storm which is an overactivation of the immune system which leads to cellular damage.16
- Continue to exercise. Do not over-exercise.
o Over-exercising temporarily reduces your immunity.17
o Engage in your routine of moderate exercise.
- Optimize your sleep especially if you have been neglecting this lately.
o Sleep and immunity are bidirectionally linked. Immune system activation alters sleep, and sleep in turn affects the innate and adaptive arm of our body's defense system.18
- Practice social distancing.
o Stop going to group classes.
o Do not gather in groups.
- Practice meticulous hygiene.
o Wash your hands often.
o Do not touch your face.
o If others visit, sanitize all commonly touch surfaces.
- Wear a mask when going out to public areas.
o This is controversial because we need these masks for healthcare professionals who are treating patients and there is a limited supply world-wide. The media will continue to state that masks will not protect you because we do not want the public to take/utilize masks that are necessary for life saving procedures and interventions. If you have a mask already, use it.
o The mask protects against droplet transmission and cough transmission. It also reminds you not to touch your face.
o The mask protects others from you.
- Limit your visits to loved ones who are at risk.
o Do not visit if you don’t have to.
o If you do visit, practice contact precautions.
o If you are taking care of a loved one who is at risk, practice meticulous hygiene and contact precautions- use a mask, wash your hands, do not touch your face.
What to plan for
- Practice social distancing but do things that you need to do that don’t involve large groups of people because this may be for the long haul.
- Government imposed quarantine may occur in the next 1-2 weeks, if not longer.19,12
o The next 1-2 weeks is a critical period where the pandemic may peak in the US.
- You will likely become infected with SARS-CoV2 and have either no symptoms or mild disease.20
o Harvard Epidemiologist Marc Lipsitch has estimated that 40-70% of the world’s population may become infected.
What to do if you get sick or catch SARS-CoV2
- If you are sick, you likely do not have COVID-19. More than likely, you have the common cold or the flu. Nonetheless, you must practice good hygiene so you are not infecting others. Wear a mask. Wash your hands often. Do not touch your face. Isolate yourself as much as possible from your family in your room.
- The mean incubation period for SASRS-CoV2 to disease presentation is 6.4 days.9
- Among hospitalized patients, fever is the most common symptom, followed by cough.5,8,9
o Fever (92-98%)
o cough (75-76%)
o myalgia/fatigue (44-75%)
o gastrointestinal symptoms (3-40%)
o It is important to note that we do not know the rates and manifestation of symptoms in non-hospitalized people with mild disease.
- Take your temperature twice a day. If your temperature is under 100.4 degrees F, you are less likely to have COVID-19.
o Subjective chills constitute fever for COVID-19.
o Temperature <100.4 degrees F – continue to monitor twice a day until cold/flu symptoms subside.
o Temperature 100.4-101.4 degrees F – take your temperature again in an hour. If temperature is sustained over an hour without resolution, you have a fever and need to monitor your temperature every 4-6 hours and monitor for signs of shortness of breath.
o Temperature 101.4 degrees F is a definitive fever. Record your temperature and monitor every 4-6 hours and monitor for signs of shortness of breath.
- If you develop shortness of breath, call your doctor immediately or put on a mask and go to the ER.
o Avoid touching your face or anyone else to limit infecting others.
o If you are taking a friend or family member to the ER, put on a mask so you do not infect others.
- If you have a fever and mild disease, isolate yourself for 14 days from the onset of symptoms or for 3 days after the resolution of symptoms (whichever is longer).1
o The likely incubation time is much shorter and 14 days is likely an over-estimate, but there is still much we don’t know about this virus.21
o Drink warm fluids, manage your symptoms, take your supplements, rest, relax, and recover.
- At the time of this letter, if you are not at high risk, you do not need to get tested. This may change as more commercially available tests become widely available in the coming days.
o We do not currently have enough kits and if you are not critically ill, we need these kits and healthcare capacity for those who are critically ill.
o The sensitivity of the test (quantitative RT-PCR analysis) is poor - anywhere between 30-68% for a variety of reasons including lack of understanding of what body region to swap, differences in viral loads of patients, and lack of gold standard.19
o Given the low sensitivity, testing negative does not mean you don’t have the virus.
o Given the low sensitivity, please consider if you really want to go into a high traffic area populated by sick individuals and exposure yourself to SARS-CoV2 if you have not contracted the virus.
Treatments in the Works
- Flattening the curve and social distancing allows us to find treatments that work. The longer you delay your exposure to SARS-CoV2, the more likely it is that treatments will be better elucidated by the time you are exposed.1
- Angiotensin receptor blockers: A few weeks ago this was thought to be helpful,22 but no longer is the case. Stay on your ACE-inhibitors, ARB (Losartan, Valsartan, etc.) or blood pressure medications unless directed by your doctor.
- Antibody therapy intervention: The strategy takes antibodies from individuals that have been infected and have since recovered to treat those who are severely ill. Arturo Casadevall and colleagues at John Hopkins University have already started testing this therapy.23
- Antiviral: Antiviral drugs like Remdesivir work against RNA viruses like coronavirus. The drug has moved in phase 3 trial in the US, Europe, and China. 9,24
- Chloroquine: The virus may be susceptible to chloroquine through changes to the lysosomal pH. As of this moment, this is the drug of choice being used in critically ill patients in conjunction with Remdesivir.9,25
- Vaccines: Vaccines will take 2-3 years to develop because of multiphase trials and risk of immune enhancement where vaccines make response to viruses even worse. This was seen in the early development of the Respiratory syncytial virus (RSV) vaccine.26
References:
1. Centers for Diseae Control and Prevention. Coronavirus Disease 2019 (COVID-19): Information for Healthcare Professionals. https://www.cdc.gov/coronavirus/2019-ncov/hcp/index.html.
2. Wong A, Li X, Lau S, Woo P. Global Epidemiology of Bat Coronaviruses. Viruses. 2019;11(2):174. doi:10.3390/v11020174
3. Fan Y, Zhao K, Shi Z-L, Zhou P. Bat Coronaviruses in China. Viruses. 2019;11(3). doi:10.3390/v11030210
4. Li W, Zhang C, Sui J, et al. Receptor and viral determinants of SARS-coronavirus adaptation to human ACE2. EMBO J. 2005;24(8):1634-1643. doi:10.1038/sj.emboj.7600640
5. Chen C, Zhou Y, Wang DW. SARS-CoV-2: a potential novel etiology of fulminant myocarditis. Herz. March 2020. doi:10.1007/s00059-020-04909-z
6. Young BE, Ong SWX, Kalimuddin S, et al. Epidemiologic Features and Clinical Course of Patients Infected With SARS-CoV-2 in Singapore. JAMA. March 2020. doi:10.1001/jama.2020.3204
7. Cao Q, Chen Y-C, Chen C-L, Chiu C-H. SARS-CoV-2 infection in children: Transmission dynamics and clinical characteristics. Journal of the Formosan Medical Association. 2020;119(3):670-673. doi:10.1016/j.jfma.2020.02.009
8. Zhang J, Dong X, Cao Y, et al. Clinical characteristics of 140 patients infected with SARS‐CoV‐2 in Wuhan, China. Allergy. February 2020:all.14238. doi:10.1111/all.14238
9. Lai C-C, Shih T-P, Ko W-C, Tang H-J, Hsueh P-R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. International Journal of Antimicrobial Agents. 2020;55(3):105924. doi:10.1016/j.ijantimicag.2020.105924
10. van Doremalen N, Bushmaker T, Morris D, et al. Aerosol and Surface Stability of HCoV-19 (SARS-CoV-2) Compared to SARS-CoV-1. Infectious Diseases (except HIV/AIDS); 2020. doi:10.1101/2020.03.09.20033217
11. Ong SWX, Tan YK, Chia PY, et al. Air, Surface Environmental, and Personal Protective Equipment Contamination by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) From a Symptomatic Patient. JAMA. March 2020. doi:10.1001/jama.2020.3227
12. Peter Hotez MD PhD. https://peterhotez.org.
13. Li R, Lipstich M, Rivers C. The demand for inpatient and ICU beds for COVID-19 in the US: lessons from Chinese cities. March 2020.
14. Secor SM, Carey HV. Integrative Physiology of Fasting. In: Terjung R, ed. Comprehensive Physiology. Hoboken, NJ, USA: John Wiley & Sons, Inc.; 2016:773-825. doi:10.1002/cphy.c150013
15. Federal Trade Commission. Coronavirus Scam. Consumer Information. https://www.consumer.ftc.gov/features/coronavirus-scams-what-ftc-doing.
16. Fu Y, Cheng Y, Wu Y. Understanding SARS-CoV-2-Mediated Inflammatory Responses: From Mechanisms to Potential Therapeutic Tools. Virol Sin. March 2020. doi:10.1007/s12250-020-00207-4
17. Walsh NP. Recommendations to maintain immune health in athletes. European Journal of Sport Science. 2018;18(6):820-831. doi:10.1080/17461391.2018.1449895
18. Besedovsky L, Lange T, Haack M. The Sleep-Immune Crosstalk in Health and Disease. Physiological Reviews. 2019;99(3):1325-1380. doi:10.1152/physrev.00010.2018
19. County of Los Angeles Public Health. Clinical Update II on Coronavirus Disease 2019. Presented at the: March 13, 2020. http://publichealth.lacounty.gov/cme/CoVWebinar/.
20. Shaw J. Cooperating to Combat Coronavirus. Harvard Magazine. March 2020. https://harvardmagazine.com/2020/03/fighting-sars-2.
21. Jiang X, Rayner S, Luo M. Does SARS‐CoV‐2 has a longer incubation period than SARS and MERS? J Med Virol. February 2020:jmv.25708. doi:10.1002/jmv.25708
22. Gurwitz D. Angiotensin receptor blockers as tentative SARS‐CoV‐2 therapeutics. Drug Dev Res. March 2020:ddr.21656. doi:10.1002/ddr.21656
23. Could a serum prevent coronavirus? A Johns Hopkins immunologist explores the idea. https://hub.jhu.edu/2020/03/03/casadevall-coronavirus-serum/. Published March 3, 2020.
24. Hoffmann M, Kleine-Weber H, Schroeder S, et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell. March 2020:S0092867420302294. doi:10.1016/j.cell.2020.02.052
25. Colson P, Rolain J-M, Raoult D. Chloroquine for the 2019 novel coronavirus SARS-CoV-2. International Journal of Antimicrobial Agents. 2020;55(3):105923. doi:10.1016/j.ijantimicag.2020.105923
26. Hurwitz JL. Respiratory syncytial virus vaccine development. Expert Review of Vaccines. 2011;10(10):1415-1433. doi:10.1586/erv.11.120
The content on this newsletter is for educational purposes only and should not be used as a substitute for medical advice. Please consult with your healthcare provider prior to initiating treatments.






