What is Fascial Layer Specific Hydromanipulation (FLuSH) Technique?
Fascial Layer Specific Hydromanipulation (FLuSH) is a novel technique developed by Dr. Wang to diagnose and treat myofascial pain. The FLuSH technique involves using ultrasound guidance to inject approximately 0.5 mL of normal saline into a specific fascial layer of the myofascial unit. The term “hydromanipulation” differentiates this technique from “hydrodissection”, a technique used to treat nerve entrapments. The pressure of the injectate is used to open the deep fascia from the superficial fascia and the underlying muscle. In the deep fascia, the same process is repeated with the needle targeting the hypoechoic extracellular matrix layers between organized fascia layers. The injectate is used to incrementally separate the soft tissues in front of the needle. In the muscle and superficial fascia, a similar process is used to disperse saline to dilute aggregates in areas of stiffness corresponding to changes that are seen under elastography.
The published results are reported in the peer reviewed medical journal Medicina: Myofascial Injection Using Fascial Layer-Specific Hydromanipulation Technique (FLuSH) and the Delineation of Multifactorial Myofascial Pain
Background and objectives:
The aims of this study were to delineate the contribution of specific fascial layers of the myofascial unit to myofascial pain and introduce the use of ultrasound-guided fascial layer-specific hydromanipulation (FLuSH) as a novel technique in the treatment of myofascial pain. Materials and Methods: The clinical data of 20 consecutive adult patients who underwent myofascial injections using FLuSH technique for the treatment of myofascial pain were reviewed.
The FLuSH technique involved measuring the pain pressure threshold using an analog algometer initially and after each ultrasound guided injection of normal saline into the specific layers of the myofascial unit (superficial fascia, deep fascia, or muscle) in myofascial points corresponding with Centers of Coordination/Fusion (Fascial Manipulation®). The outcome measured was the change in pain pressure threshold after injection of each specific fascial layer. Results: Deep fascia was involved in 73%, superficial fascia in 55%, and muscle in 43% of points. A non-response to treatment of all three layers occurred in 10% of all injected points. The most common combinations of fascial layer involvement were deep fascia alone in 23%, deep fascia and superficial fascia in 22%, and deep fascia and muscle in 18% of injected points. Each individual had on average of 3.0 ± 1.2 different combinations of fascial layers contributing to myofascial pain.
Conclusions: The data support the hypothesis that multiple fascial layers are responsible for myofascial pain. In particular, for a given patient, pain may develop from discrete combinations of fascial layers unique to each myofascial point. Non-response to treatment of the myofascial unit may represent a centralized pain process. Adequate treatment of myofascial pain may require treatment of each point as a distinct pathologic entity rather than uniformly in a given patient or across patients.
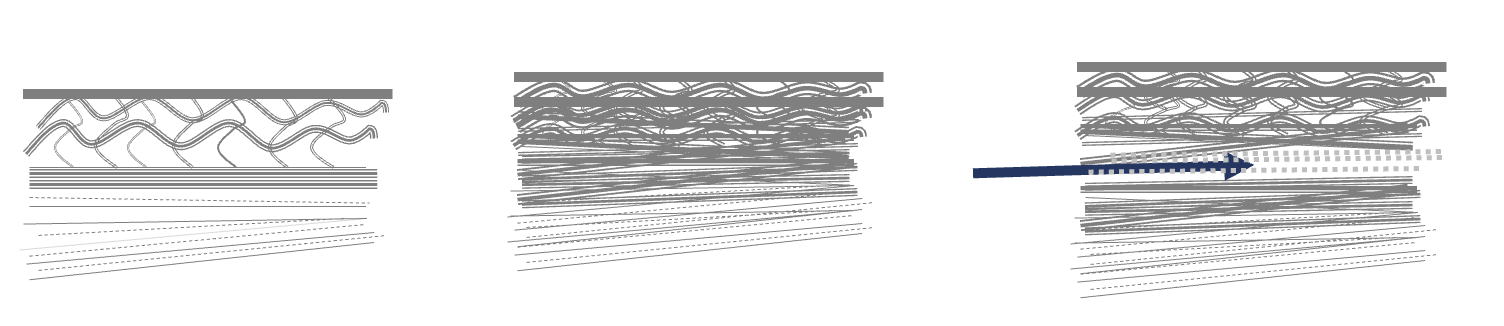
Normal Fascia | Densification of Fascia | Fascial Layer Specific Hydromanipulation








