What is Pelvic Floor Dysfunction?
Pelvic Floor Dysfunction (PFD) is defined by the International Pelvic Pain Society as a condition when the pelvic floor muscles do contract, relax, or work together. The pelvic floor is made up of bones, muscles, fascia, and ligaments and functions as a hammock to support the pelvic organs including the uterus, bladder, and rectum. If the muscles become overactive, strained or uncoordinated, they may cause pain in the pelvis. This pain may lead the muscles to not contract, relax, or work together.
Pelvic Floor Dysfunction and HSD / hEDS
Pelvic floor dysfunction is highly prevalent among individuals with Hypermobility Spectrum Disorders (HSD)/ hypermobile Ehlers-Danlos syndrome (hEDS). The high incidence of pelvic floor symptoms in this population significantly impacts urinary and fecal continence, pelvic organ support, and overall quality of life.
Connective tissue disorders like hEDS contribute to the pathogenesis of pelvic floor dysfunction. Cisgender women with hEDS report a high prevalence of pelvic floor symptoms, including stress urinary incontinence (60%), urgency urinary incontinence (54%), fecal incontinence (24%), and pelvic organ prolapse (21%).[1] Bladder symptoms are particularly bothersome, and pelvic pain is reported by 71% of people with hEDS. A study comparing hEDS and Marfan syndrome (MFS) patients found that 50% of women with hEDS reported urinary incontinence, and 75% reported pelvic organ prolapse, indicating a higher prevalence of these symptoms compared to women with MFS.[2] Additionally, anorectal manometry studies have shown that patients with hEDS exhibit altered anorectal pressure profiles, including less anal relaxation and higher residual anal pressures during simulated defecation, which may contribute to impaired rectal evacuation.[3]
Reference:
1. Pelvic Floor Symptoms in Cisgender Women With Ehlers-Danlos Syndrome: An International Survey Study.
Kciuk O, Li Q, Huszti E, McDermott CD. International Urogynecology Journal. 2023;34(2):473-483. doi:10.1007/s00192-022-05273-8.
2. Urinary Incontinence and Pelvic Organ Prolapse in Women With Marfan or Ehlers Danlos Syndrome.
Carley ME, Schaffer J. American Journal of Obstetrics and Gynecology. 2000;182(5):1021-3. doi:10.1067/mob.2000.105410.
3. Anorectal Manometry for the Diagnosis of Pelvic Floor Disorders in Patients With Hypermobility Spectrum Disorders and Hypermobile Ehlers-Danlos Syndrome. Zhou W, Zikos TA, Halawi H, et al. BMC Gastroenterology. 2022;22(1):538. doi:10.1186/s12876-022-02572-8.
What are the muscles of the pelvic floor?
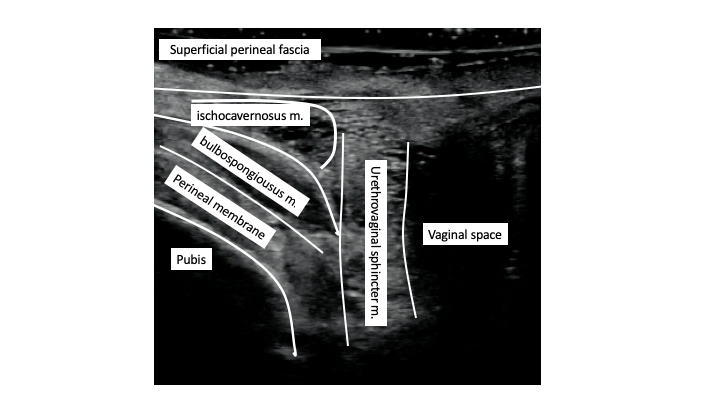
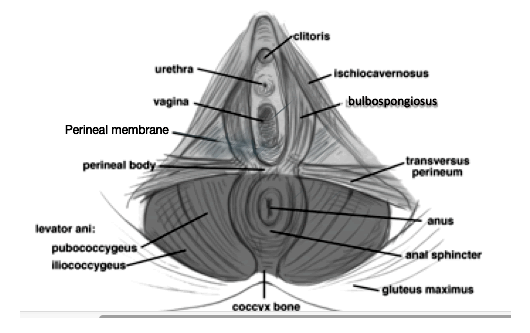
The anterior aspect of the pelvic floor is not well characterized. The entire posterior pelvic floor is referred to collectively referred to as the levator ani, it includes the pubococcygeus, puborectalis, and iliococcygeus. The anterior pelvic floor surrounding the vaginal opening include the bulbospongiosus, ischiocavernosus, transverse perineal muscle, the anterior attachments of the pubococcygeus, perineal membrane, and superficial perineal fascia.
Reference:
Kruger JA, Murphy BA, Heap SW. Alterations in levator ani morphology in elite nulliparous athletes: a pilot study. Aust. N. Z. J. Obstet. Gynaecol. 2005; 45:42-7.
Elastography study
Pelvic pain and pelvic floor dysfunction are highly prevalent in female athletes, including dancers. Hypertonicity of the pelvic floor can be a contributing factor.
The purpose of the study was to objectively demonstrate the presence of pelvic floor stiffness and dysfunctional movement using real-time sonoelastography.
Real-time sonoelastography was used to examine the pelvic floor complex in four female subjects, approximately 40-years-old: 1 dancer and 1 non-dancer with pelvic floor dysfunction, 1 dancer and 1 non-dancer without pelvic floor dysfunction. Transperineal dynamic ultrasound of the pelvic floor of 4 participants were conducted using B- mode and elastography. Transperineal dynamic ultrasound of the pelvic floor of the 4 participants were conducted using B-mode and elastography to evaluate fascial tissue quality and stiffness. The relative velocities of inter-fascial plane movement were calculated and the quality of inter-fascial plane gliding was evaluated using Echolizer ver 1 (GLAB Corp, Hiroshima, Japan) software.
Elastography showed increased stiffness in the bulbospongiosus, superficial transverse perineal, and puborectalis muscles in patients with pelvic dysfunction compared to those without pelvic floor dysfunction. Pelvic floor stiffness and atrophy are notable in the hypermobile dancer with pelvic pain. Subjects with pelvic pain had lower relative
velocity between fascial planes compared with their counterparts without pain. The non-dancer with pelvic dysfunction demonstrated the most total motion, and the dancer with pelvic floor dysfunction demonstrated no inter fascial-plane movement.
References:
Wang TJ, Winder B, Cordova-Caddes A, Gamada K. Pelvic floor stiffness in pelvic floor dysfunction of dancers vs. non-dancers. 10th Interdisciplinary World Congress on Low Back and Pelvic Girdle Pain; 2019 Oct 28-31; Antwerp, Belgium.
What are the types of pelvic floor dysfunction?
PFD is broadly categorized into 2 types: hypotonic PFD and hypertonic PFD.
Hypotonic PFD is more common, presenting with urinary incontinence, fecal incontinence, or pelvic organ prolapse.
The less common of the two types is hypertonic PFD> Hypertonic PFD symptoms include impaired ability to evacuate urine or stool, sexual dysfunction, and pelvic pain. In this disorder, muscles of the pelvic floor remain in a contracted state causing increased pressure and pain. The pain is persistent and typically worsens throughout the day and with daily activities, such as walking, physical activity, and passing stool. This is anecdotally seen more commonly in gymnasts, dancers, and high-stress professions.
References:
Louis-Charles K, Biggie K, Wolfinbarger A, Wilcox B, Kienstra CM. Pelvic Floor Dysfunction in the Female Athlete. Curr Sports Med Rep. 2019 Feb;18(2):49-52.
Faubion SS, Shuster LT, Bharucha AE. Recognition and management of nonrelaxing pelvic floor dysfunction. Mayo Clin. Proc. 2012; 87:187-93.
Butrick CW. Pathophysiology of pelvic floor hypertonic disorders. Obstet. Gynecol. Clin. N. Am. 2009; 36:699-705.
How is PFD treated?
Soft tissue mobilization of fascial adhesions like Thiele massage can address pelvic pain symptoms, as well as bladder and bowel dysfunction. Movement rehabilitation including lumbopelvic stabilization and core strengthening are critical in resolution of symptoms.
References:
Weiss JM. Pelvic floor myofascial trigger points: manual therapy for interstitial cystitis and the urgency-frequency syndrome. J. Urol. 2001; 166:2226-31.
Pastore EA, Katzman WB. Recognizing myofascial pelvic pain in the female patient with chronic pelvic pain. J. Obstet. Gynecol. Neonatal. Nurs. 2012; 41:680-91.
Montenegro ML, Vasconcelos EC, Candido Dos Reis FJ, et al. Physical therapy in the management of women with chronic pelvic pain. Int. J. Clin. Pract. 2008; 62:263-9. S







